Heart Department
When it comes to heart care, we have a multidisciplinary team who specialise in preventing, diagnosing and resolving cardiovascular problems, however complicated they may be.



Heart Department
Our Heart Department is both staffed by a medical team with extensive experience in the diagnosis and treatment of coronary and cardiac diseases which can be treated percutaneously, and equipped with cutting-edge high technology, since we have hybrid operating theatres where surgeries on structural cardiac conditions are performed to the highest safety standards.
The Cardiac Surgery Unit has been a leader in the surgical treatment of adult cardiac disease for more than 15 years, and the members of the cardiac surgery group have performed open-heart surgery on more than 5,000 patients with outstanding outcomes. We seek to deliver the best surgical solutions, including for people who have been rejected by other hospitals or who require very complex surgery because they are high and very high risk patients.
Our Smart Cardiac Surgery Program involves a stringent quality control of the highest standards throughout the surgical procedure (preoperative, intraoperative and postoperative), which makes it one of the most advanced cardiac surgery protocols available today worldwide. A highly experienced team of heart specialists works using a holistic multidisciplinary process, which is based on the highly sought after patient-centered approach.
The Smart Cardiac Surgery Program includes beating heart coronary surgery, minimally invasive cardiac surgery, bloodless cardiac surgery and fast-track recovery.
Our program is governed by the most rigorous and disciplined practices of healthcare quality management, focused on providing the best patient care and satisfaction with maximum safety.
- Our team is committed to excellence and our goal is to provide the best care to our patients and their families.
- At present, cardiac surgery can be performed with minor surgical aggression, with excellent results and a very low risk for the patient.
Our Interventional Cardiac Haemodynamics Unit has an experienced team of professionals who use next-generation technology to diagnose and treat coronary and cardiac conditions. We conduct high-precision studies in state-of-the-art laboratories. In recent years, haemodynamics has developed percutaneous techniques to treat aortic and mitral valve conditions (percutaneous aortic valve prosthesis, leak closures) or congenital malformations (fixing short circuits), that just a few years ago, needed surgical correction. We can deal with more and more conditions without the need for open surgery. Without doubt, the ideal environment for carrying out this type of treatments is the hybrid operating theatre, which unites the sterile conditions of the surgical environment with the most advanced X-ray technology. Without doubt, the ideal environment for performing this type of treatments is the hybrid operating theatre, which unites the sterile conditions of the surgical setting with the most advanced X-ray technology. During the procedures, we also add the overlapping of images taken by other techniques (ultrasound, echocardiography, Echo Navigator, CT scan, and Heart Navigator) for better precision.
- We have a hybrid operating theatre, which unites the sterile conditions of the surgical environment with the most advanced X-ray technology.
-
For the diagnosis and treatment of coronary heart disease, we conduct high-precision studies in state-of-the-art laboratories.
With over 35 years’ experience and over 10,000 heart defects operated, our team of specialists deals with all types of congenital heart defects from neonatal age to adults with congenital problems. 70% of the heart defects that we treat are complex, with an Aristotle Basic Score of 8.2, which is higher than the European average, and with a survival rate of 98.2%.
- Over 10,000 heart defects operated, 70% of which are of maximum complexity. We operate on all kinds of heart defects, including those in Group 4 of the Aristotle Basic Score
- Personalised care with a 1:1 doctor-patient relationship
- International experts for complex congenital heart defects. We provide medical assistance to patients from several countries.
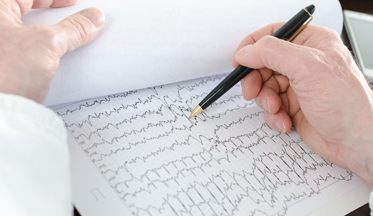
Our arrhythmia experts conduct electrophysiological studies with high-performance equipment for diagnostic and therapeutic purposes. They treat patients that have been previously diagnosed and referred by Cardiology or Internal Medicine specialists to the Electrophysiology and Arrhythmias Department for treatment.
Our specialists perform ablations, arrhythmia studies, pacemaker implant and monitoring treatments, electric cardioversion, tilt table tests to study syncope, as well as arrhythmia Holter monitoring and pressure Holter monitoring
- Some of our centres perform the most ablations to treat atrial fibrillation, with a higher volume than some of the country’s main centres.
- Thanks to our experience and the use of next-generation technology, we provide a personalised and precise medicine.