قسم أمراض القلب
من أجل رعاية قلبك، لدينا فريق متعدد التخصصات متخصص في تفادي حدوث أي مشكلة في القلب والأوعية الدموية، وتشخيص هذا النوع من الأمراض ومعالجته، مهما بلغت درجة التعقيد.



قسم أمراض القلب
يضم قسم أمراض القلب لدينا، من ناحية، فريقًا طبيًا ذا خبرة طويلة في مجال تشخيص أمراض الشرايين التاجية والقلب وعلاجها والتي يمكن معالجتها عن طريق الجلد؛ ومن ناحية أخرى، تتوفر لدينا أحدث التكنولوجيا، فيوجد غرف عمليات هجينة حيث نجري العمليات في مجال أمراض القلب الهيكلية مع الحفاظ على أعلى معايير السلامة.
تعتبر وحدة جراحة القلب رائدة في العلاج الجراحي لأمراض القلب لدى البالغين منذ أكثر من 15 عامًا، وقد أجرى أعضاء مجموعة جراحة القلب جراحة مفتوحة لأكثر من 5000 مريض، وكانت النتائج رائعة. نحن نسعى لتقديم أفضل الحلول الجراحية، بما في ذلك المرضى الذين رفضتهم مستشفيات أخرى أو الذين يحتاجون إلى عملية جراحية معقدة للغاية لأن حياتهم في حالة خطرة أو خطرة للغاية.
يتضمن برنامج جراحة القلب الذكي لدينا مراقبة صارمة للجودة بأعلى المعايير في جميع مراحل العملية الجراحية (ما قبل الجراحة وأثناء العملية وبعد العملية الجراحية)، مما يجعله واحدًا من بروتوكولات جراحة القلب الأكثر تقدمًا المتوفرة اليوم في جميع أنحاء العالم. يعمل فريق من أخصائيي القلب من ذوي الخبرة العالية باستخدام عملية شاملة متعددة التخصصات، والتي تعتمد على النهج المرغوب فيه للغاية والمتمحور حول المريض.
يشتمل برنامج جراحة القلب الذكية على جراحة القلب النابض لتوصيل الشرايين التاجية وجراحة القلب ذات الحد الأدنى من التدخل، وجراحة القلب بلا دماء، والتعافي السريع.
يخضع برنامجنا للممارسات الأكثر صرامة والمنضبطة لإدارة جودة الرعاية الصحية، التي تركز على تقديم أفضل رعاية صحية وتستهدف إرضاء المرضى مع أقصى درجات السلامة.
- يلتزم فريقنا بالسعي إلى تحقيق التميز، وهدفنا هو تقديم أفضل رعاية لمرضانا وأسرهم.
- في الوقت الحاضر، يمكن إجراء جراحة القلب عن طريق تقنية الحد الأدنى من التدخل الجراحي، مع الحصول على نتائج ممتازة ومخاطر منخفضة للغاية بالنسبة للمريض.
تضم وحدة ديناميكا الدم-طب القلب التدخلي فريقًا من ذوي الخبرة من المهنيين الذين لديهم أحدث التقنيات لتشخيص أمراض القلب والشريان التاجي وعلاجها. نحن نجري دراسات عالية الدقة في مختبرات مجهزة بأحدث التقنيات. وخلال السنوات الأخيرة، طورت وحدة ديناميكا الدم تقنيات عن طريق الجلد لعلاج أمراض الصمام الأبهري والتاجي (قسطرة الأبهر عن طريق الجلد، إغلاق التسربات) أو التشوهات الخلقية (إغلاق التحويلات) التي كانت تتطلب تصحيحًا جراحيًا قبل بضع سنوات. أصبحت الأمراض التي يمكننا معالجتها دون الحاجة لإجراء عملية جراحية مفتوحة تتزايد أكثر فأكثر. ومما لا شك فيه فإن البيئة المثالية لتنفيذ هذا النوع من العلاج هي غرفة العمليات الهجينة التي تجمع بين ظروف التعقيم في البيئة الجراحية وتقنية أشعة إكس الأكثر تطورًا. ولمزيد من الدقة، نضيف أيضًا خلال الإجراءات تراكب الصور التي توفرها تقنيات أخرى (الموجات فوق الصوتية-تخطيط صدى القلب-Echo Navigator-الأشعة المقطعية -Heart Navigator-).
- -لدينا غرفة عمليات هجينة تجمع بين ظروف التعقيم في البيئة الجراحية وتقنية أشعة إكس الأكثر تطوراً.
- من أجل تشخيص وعلاج مرض الشريان التاجي، فإننا نجري دراسات عالية الدقة في مختبرات مجهزة بأحدث التقنيات.
لدينا فريق من المتخصصين، الذين يتمتعون بخبرة تزيد عن 35 عامًا وأجروا أكثر من 10000 عملية جراحية في القلب، ويعالجون كافة أنواع أمراض القلب الخلقية بدءًا من حديثي الولادة وحتى الأمراض الخلقية لدى الكبار. 70% من أمراض القلب التي يعالجونها هي أمراض معقدة، حيث بلغت درجة التعقيد Aristotles Basic Score 8,2، وهي أعلى من المتوسط الأوروبي، ونسبة البقاء على قيد الحياة بعد إجراء العمليات الجراحية 98,2%.
- أكثر من 10000 عملية جراحية في القلب، 70% منها في غاية التعقيد. نجري جميع أنواع العمليات الجراحية لعلاج أمراض القلب، بما في ذلك الأمراض التي تندرج تحت المجموعة 4 من Aristotles Basic Score.
- نقدم رعاية مخصصة، وتبلغ نسبة الطبيب إلى المريض 1:1
- نمتلك الريادة الدولية لعلاج أمراض القلب الخلقية المعقدة. نقدم الرعاية الطبية إلى المرضى القادمين من عشرات البلدان.
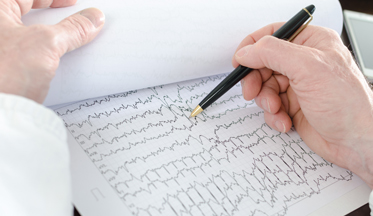
يجري خبراؤنا في مجال عدم انتظام ضربات القلب دراسات الفيزيولوجيا الكهربية لأغراض التشخيص والعلاج باستخدام معدات عالية الأداء. ويعالجون المرضى الذين سبق تشخيصهم في استشارة أمراض القلب أو الطب الباطني وأحالهم هؤلاء المتخصصون إلى قسم الفيزيولوجيا الكهربية وعدم انتظام ضربات القلب لتلقي العلاج.
يجري المتخصصون عمليات اجتثاث، ودراسات عدم انتظام ضربات القلب، والعلاج بالزراعة ومتابعة جهاز تنظيم ضربات القلب، وتقويم نظم القلب بالصدمة الكهربائية، واختبار الإمالة لدراسة الإغماء بسبب عدم انتظام ضربات القلب، بالإضافة إلى فحص هولتر لمراقبة عدم انتظام ضربات القلب وفحص هولتر لمراقبة ضغط الدم.
- لدينا بعض المراكز التي تجري عمليات الاجتثاث لعلاج الرجفان الأذيني، بقدر أكبر من تلك العمليات التي تُجرى في المراكز الرئيسية في البلاد.
- بفضل خبرتنا واستخدام أحدث التقنيات، نوفر للمرضى العلاج المخصص والدقيق.